As the AAMC Center for Health Justice prepares to host the inaugural Maternal Health Incubator later this month to address the longstanding trends of racial and ethnic health inequities for women and birthing people, hearing directly from those who have given birth is of high importance. In March and April 2022, the AAMC Center for Health Justice polled a nationally representative sample of people who gave birth in the past five years to learn about their experiences. This data brief highlights findings from the poll to provide insights about the complications and discrimination individuals have faced during pregnancy and childbirth and following childbirth and provides data for populations about whom there is limited research, such as LGBTQ+ populations.
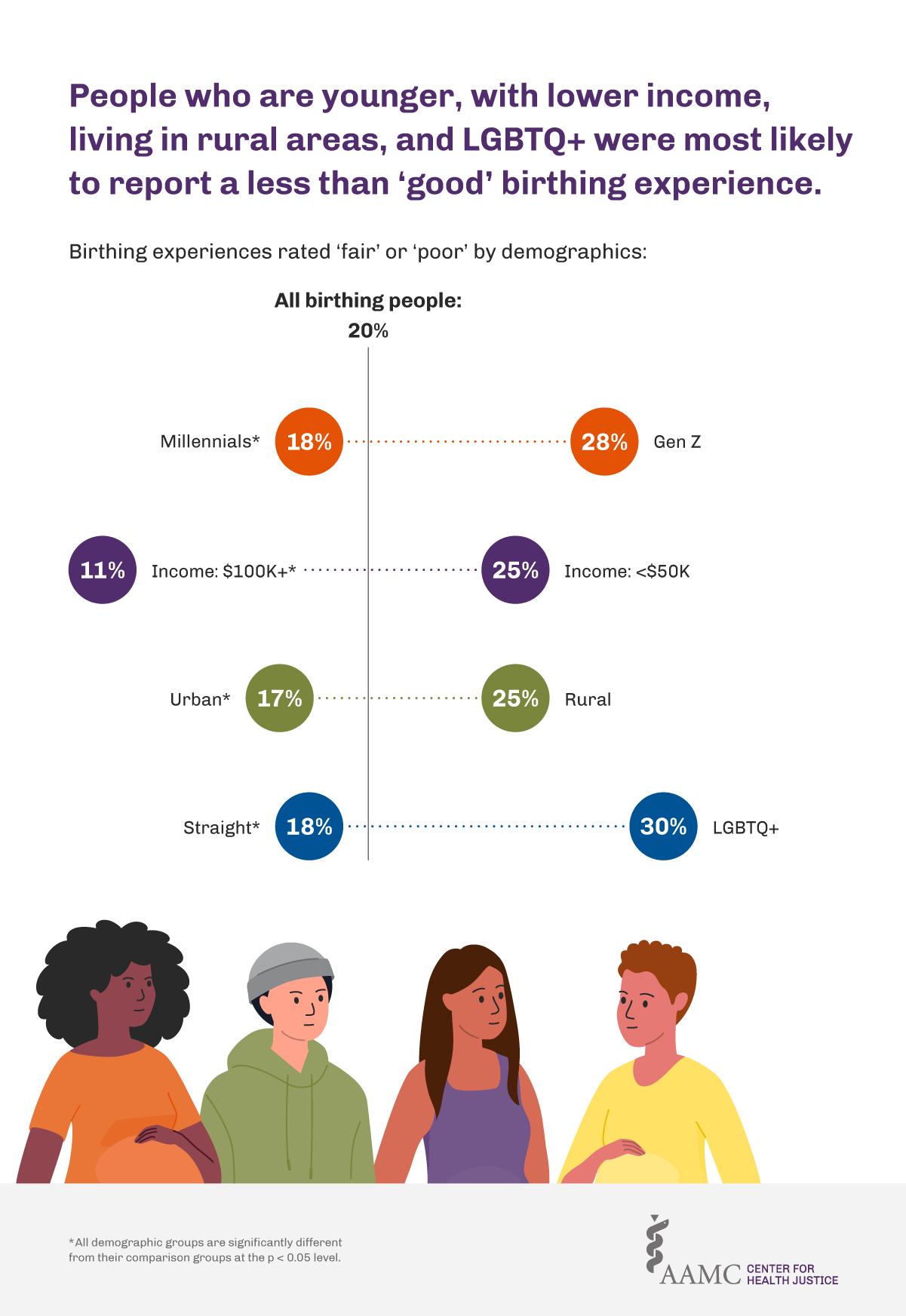
While the majority (80%) of survey respondents rated their most recent birthing experience as “excellent” or “good,” one-fifth (20%) rated their experience as “fair” or “poor.” Birthing people who are part of Generation Z (born 1997-2004), LGBTQ+, with an annual income below $50,000, or who are living in rural areas were the most likely to report fair or poor birthing experiences in the last five years (Figure 1).
Two-thirds (66%) of respondents reported some type of postpartum complication, with the largest share (38%) reporting postpartum depression and/or anxiety. Seven of ten respondents reported being screened for mental health complications, while 30% reported that they were not screened for or asked about depression or anxiety-related symptoms at any point during or after their pregnancy. However, inequities in screening were significant. Respondents who were Hispanic (62%), unemployed (60%), and with lower incomes (66%) were the least likely to be screened for mental health complications during or after their pregnancy (Figure 2).
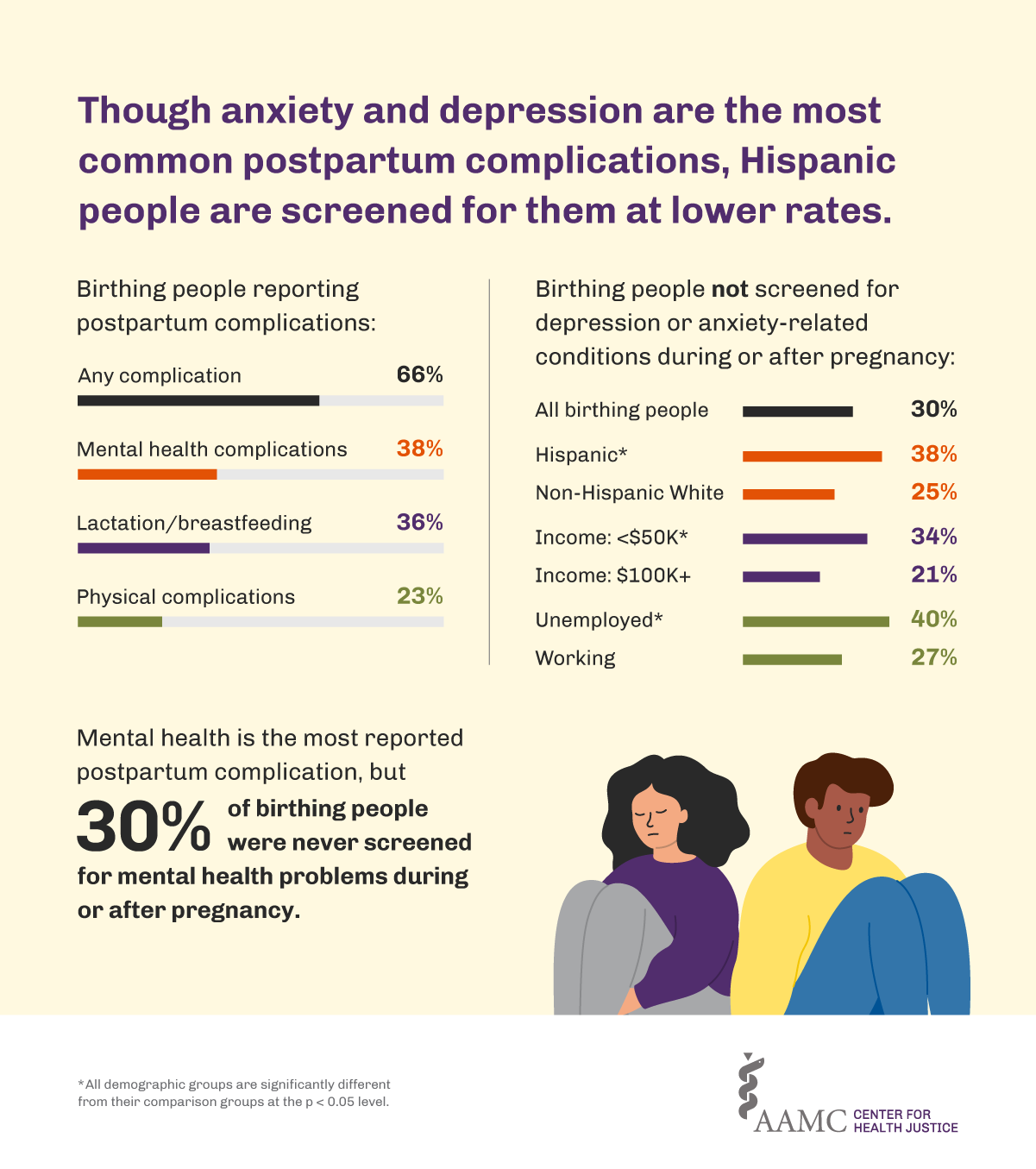
For screenings to be effective, people need to be able to trust their health care providers and the organizations that provide them care and need to feel comfortable sharing information about their mental health, given its sensitive nature. Previous polling by the center has found that those made most vulnerable to health inequities were also more likely to have reservations about sharing their personal health information. Any interventions to address maternal health inequities should include efforts to become trustworthy partners to birthing people and their communities.
The COVID-19 pandemic also presented distinct challenges for pregnancy and childbirth: not being able to have visitors for appointments or the birthing process, fear for their child’s health, lack of social support, limited availability of pre- and postnatal appointments, and difficulties with work and finances were common. Nearly half of respondents reported that their primary challenges due to COVID-19 during pregnancy, labor, and postpartum care were related to limits on the number of visitors for appointments or during the birth. One said, “I was asked to keep my mask on the entire time I was at the hospital. I was allowed no visitors and felt very isolated.” Many respondents reported negative effects on their mental health from the added burden of the pandemic.
“It made my mental health dwindle rapidly,” said another respondent.
The experiences described by participants have broader implications for poor postpartum mental health, which may have been exacerbated by the pandemic. While most respondents did not meet eligibility requirements for a COVID-19 vaccine while pregnant (62%), of those who were eligible most (60%) did not receive a vaccine. Those with a higher educational attainment were more likely to get vaccinated while pregnant. Of college-educated birthing people, 22% reported receiving a vaccine, versus 10% of those with less than a college education.
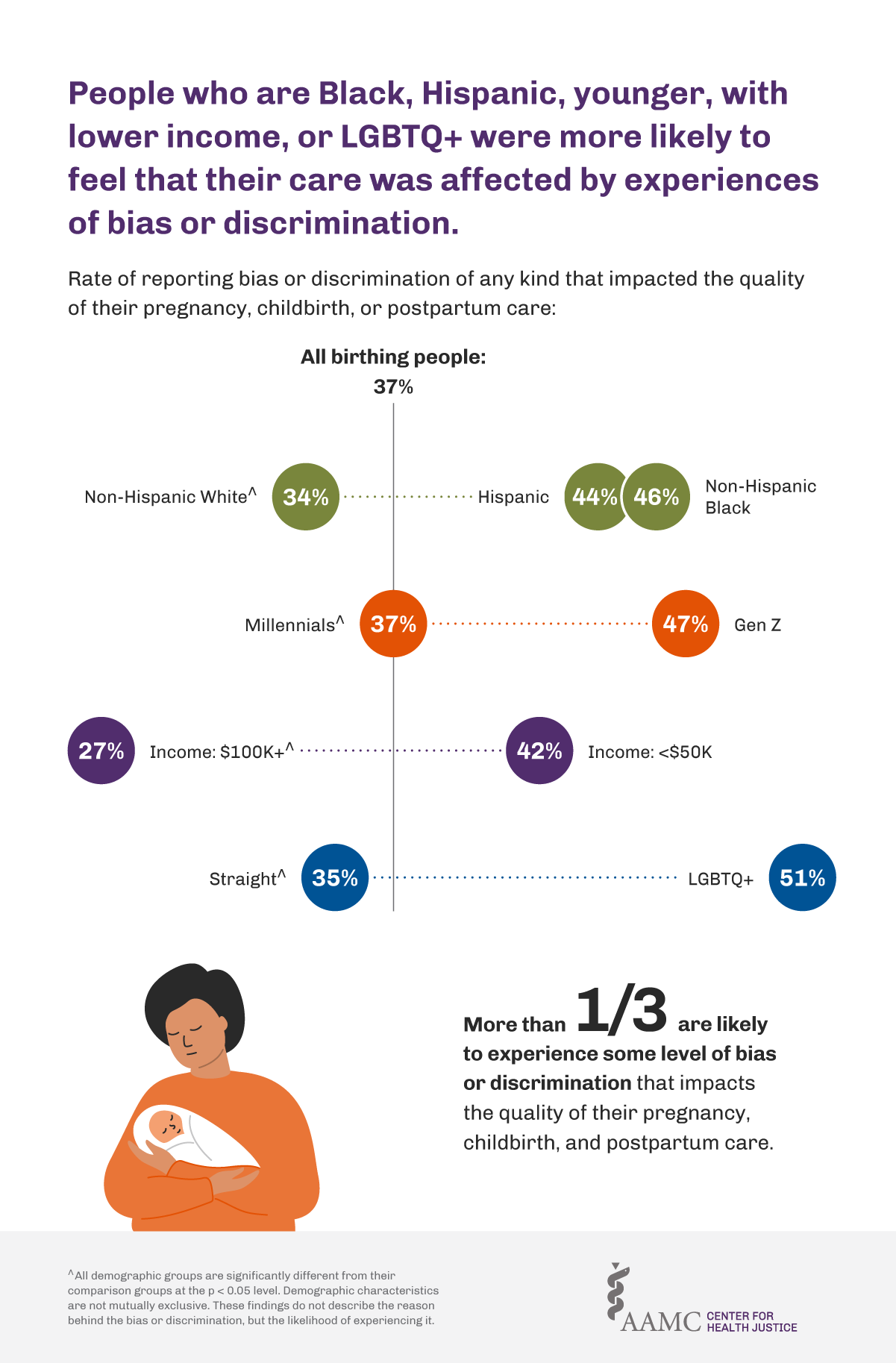
Factors other than the pandemic continued to influence the experiences of birthing people. A decline in mental health was the leading postpartum complication. Nearly one-fifth of respondents reported difficulty returning to work and almost four in ten reported no access to postpartum paid leave from work. Over one-third (37%) felt that their quality of pregnancy, birth, and postpartum care was affected by experiences of bias or discrimination. People who were Black, Hispanic, younger, with lower incomes, or LGBTQ+ were more likely than their counterparts to feel that any kind of bias or discrimination affected their birth experiences. Figure 3 shows the likelihood of experiencing bias or discrimination that influenced the quality of their pregnancy, birth, and postpartum care, though not necessarily the reasoning for bias or discrimination.
This polling aligns with the AAMC Center for Health Justice’s goal of using rigorous research and data to inform policy efforts and improve the effectiveness of programs and services for birthing people. On May 24 and 25, the center will host the Maternal Health Incubator, convening policy makers, public -health experts, clinicians, community workers, and other experts to identify evidence-based, innovative approaches for addressing maternal health inequities. One approach that will be presented at the virtual event is an upcoming examination of the impact of paid leave on health equity and the implications for policymaking.
Register now for the incubator and sign up for the Center for Health Justice newsletter to learn more as we continue to address maternal health inequities through research, policy analysis, and community engagement.